Professionals at Swift MB keep up with industry developments, credentialing trends, and payer regulations in order to retain their knowledge in the provider credentialing process. We handle all aspects of the credentialing procedure as professionals. That means we’ll handle everything that normally falls to your personnel so they may concentrate on more strategic initiatives.
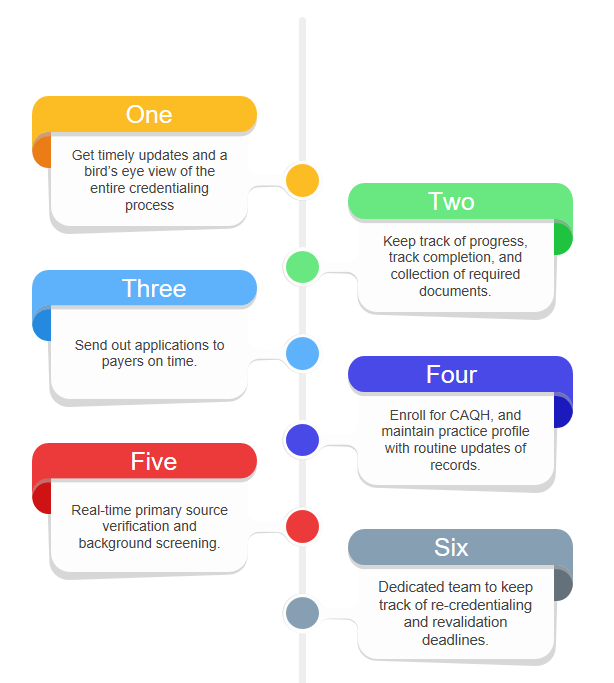
We monitor and gather all required paperwork, finish the credentialing process, submit applications to payers, and promptly address any errors or extra information requests. Each time your practise is due for re-credentialing, Swift MB will deploy a team of experts to monitor re-credentialing dates and begin, and finish, the process.
Together, our staff and the provider complete the first application, conduct primary source verification and background checks, coordinate with payers to ensure a swift approval process, and get the provider up and running as soon as possible.
Affordable and professional assistance with provider enrollment and medical credentialing is available from the team at Swift MB. There will be no more issues with cash flow or getting paid. There will be no more blunders in the data. We will eliminate all of your problems, including the risk of premature expiry. If you want to talk to us, do it now.
We assist in compiling demographic and background data for your clinic.
Oversee all verification and contact with payer organizations and other follow-up responsibilities.
Providers may rely on us for support with enrolling in CAQH and keeping their profiles updated.
Gain full access to our EHR and credentialing system so you can see what we’re up to at all times.
Make sure you have all the paperwork you need to submit your applications to the appropriate payers.
In order to make communicating with your medical organization’s credentialing process as simple as possible.
We assist in compiling demographic and background data for your clinic.
Make sure you have all the paperwork you need to submit your applications to the appropriate payers.
Gain full access to our EHR and credentialing system so you can see what we’re up to at all times.
Providers may rely on us for support with enrolling in CAQH and keeping their profiles updated.
Oversee all verification and contact with payer organizations and other follow-up responsibilities.
In order to make communicating with your medical organization’s credentialing process as simple as possible.
We assist in compiling demographic and background data for your clinic.
Providers may rely on us for support with enrolling in CAQH and keeping their profiles updated.
Make sure you have all the paperwork you need to submit your applications to the appropriate payers.
Oversee all verification and contact with payer organizations and other follow-up responsibilities.
Gain full access to our EHR and credentialing system so you can see what we’re up to at all times.
In order to make communicating with your medical organization’s credentialing process as simple as possible.